The macula is responsible for the central part of the visual field. Diseases of the macula characteristically present with reduced central vision. These diseases are summarised on this page.
Cystoid Macular Oedema (CMO)
This intraretinal oedema is s result of ocular inflammation, commonly in the post-cataract surgery phase. It can also occur in other vascular and inflammatory disorders of the eye including diabetic retinopathy, uveitis, retinitis pigmentosa and latanoprost use.
Pathology
- The mechanism of oedema is similar to elsewhere in the body, involving vessel hyper-permeability and high flow.
- The fluid gathers within the intercellular spaces of the retina, most commonly the outer plexiform layer.
- Macular oedema results in dVA because the fluid obstructs light.
Diagnostics
Presentation
- Blurry vision + metamorphopsia + scotoma
Investigation
- Diagnosis is typically made by visualisation with OCT.
- FFA can also be used and shows vessel leakage
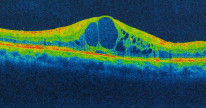
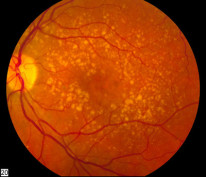
Cystoid macular oedema on OCT. By Imran kabir hossain, CC BY-SA 4.
Management
Treatment is stepwise and based on inciting injury. The mainstay is steroids.
- Firstline: NSAIDS/steroid drops
- If persisting after a month: continue topical + periorbital steroid injection (subtenon or orbital floor)
- If persisting after another month: consider intravitreal or systemic steroids
- Carbonic anhydrase inhibitors and anti-VEGF agents are used
It is important to frame the management option in context of the severity, i.e a case of mild CMO following cataract surgery should typically start with topical steroids.
Central Serous Chorioretinopathy
Central serous chorioretinopathy is an idiopathic subretinal accumulation of fluid.
Pathology
The exact mechanism is unknown but choroidal hyperpermeability is thought to play a role. This disease typically affects adult men under stress. It is also associated with steroid exposure.
Diagnostics
Presentation
- Typically a middle-aged man with a stressful occupation who presents with a sudden unilateral reduction in visual acuity and scotoma.
Investigation
- Diagnosis can be made by OCT which will show subretinal fluid collection with neurosensory retinal detachment.

A middle-aged man with a stressful job is the classic vignette for this condition.
Management
- There is a high rate of spontaneous resolution, so specific treatment is only indicated in persistent cases over months with noticeable detriment to the quality of life
- Firstline → observation for 3-6 months
- For persistent cases → micropulse laser or photodynamic therapy
- If other treatments are unsuccessful → anti-VEGF therapy may be considered
Angioid Streaks
These streaks are sections of the Bruch's membrane of the choroid that are calcified and broken.
Summary
- Bilateral symmetrical irregular atrophied streaks from the optic disc to the outer retina.
- Occur around the disc and can be visualised on FFA.
- Breaks in Bruch's membrane can lead to choroidal neovascularization which is most often the cause of visual loss in these patients
- The most common association is pseudoxanthoma elasticum where patients present with yellow papules and wrinkling of skin folds around the neck, armpits and groin: ‘plucked chicken appearance'
Systemic associations of angioid streaks can be remembered by PEPSI: Pseudoxanthoma Elasticum, Pagets, Ehlers-Danlos, Sickle cell, Idiopathic
Degenerative Myopia
The term ‘degenerative myopia’ describes progressively myopic patients (> -6D of myopia) whose axial eye length does not stabilize with age i.e a progressive myopia. This is associated with various degenerative changes.
Pathology
- A progressively lengthening eye is associated with myopia, decreased visual acuity, posterior staphyloma and breaks in Bruch's membrane ('lacquer cracks') - resulting in choroidal neovascularization and retinal detachments
- Classically associated with connective tissue disorders like Marfan syndrome and Stickler syndrome
- High myopia is a common cause of choroidal neovascularization in the young, compared to AMD in the elderly
Diagnostics
- Presentation is a young patient with high myopia and decreased visual acuity.
- Examination can show an unstably progressing axial length and the features above.
Management
- Time spent outdoors is protective
- Choroidal neovascularization → Anti-VEGF intravitreal injection