The vitreous is attached to the internal limiting membrane of the retina by collagen fibrils. Abnormalities in these attachments affect both the retina and the vitreous. The resulting diseases are discussed on this page.
Peripheral Retinal Degenerations
The majority of people have some sort of degeneration at the peripheral retina. Some of these people go on to develop breaks within the retina, which can affect vision. There are various different forms of retinal degeneration and this section will discuss the 2 most important types.
Lattice Degeneration |
Degenerative Retinoschisis |
|---|---|
Areas of vitreous liquefaction and vitreoretinal adhesion |
A microcystic area where the neurosensory retinal layers have split and formed a balloon-like pouch |
Commoner in myopes and connective tissue disorders |
Commoner in hyperopes and is typically bilateral |
On fundoscopy, characteristic zig-zag white lines around small round holes can be seen |
Typically seen on the inferotemporal region of the fundus as a smooth elevation of the retina |
Prophylactic laser retinopexy is offered to patients who have had a previous retinal detachment in the fellow eye |
Relatively lower risk of retinal detachment |
Relatively higher risk of retinal detachment |
The cyst in degenerative retinoschisis typically forms between the outer plexiform and inner nuclear layers of the retina.
Retinal Tears
Retinal tears are full-thickness breaks through the retina. Retinopexy is used as treatment in cases which are high risk for progression into retinal detachment (RD). Tears are commoner in myopic eyes, because the surface area of the retina is greater.
Description |
Risk of RD |
Treatment |
|
|---|---|---|---|
U-shaped |
|
|
|
Giant |
|
|
|
Retinal Dialysis |
|
|
|
Traumatic retinal dialysis is the commonest cause of traumatic retinal detachment in children.
Retinal Detachment
Retinal detachment is the separation of the neurosensory retina (NSR) from the retinal pigment epithelium (RPE). It is a serious condition that can lead to blindness.
Classification

Rhegmatogenous retinal detachment (commonest)
- Caused by fluid accumulation between the NSR and RPE via a break in the neurosensory retina
- Since retinal breaks are associated with PVD, signs of PVD are typically seen
Tractional retinal detachment
- Caused by adhesional vitreous traction on the retina
- Typically seen in DR and ROP
Exudative retinal detachment
- Failure of the outer blood-retinal barrier → subretinal fluid accumulation → retinal detachment
- Occurs due to lesion of the RPE including: uveitis, choroidal tumour/neovascularisation, uveal effusion syndrome
The NSR is attached to the RPE primarily by hydrostatic forces.
Diagnostics
Presentation
- Curtain-like vision loss, RAPD, Shaffer sign and Weiss ring (a sign of PVD)
Investigations
- A recent detachment will appear on fundoscopy as a dome with loss of RPE markings
- A chronic detachment will show a characteristic demarcation line
- B-scan ultrasound can be used if the view is obstructed (cataracts or vitreous haemorrhage)
- Indirect ophthalmoscopy with scleral depression is used to visualise the ora serrata
Management (depends on type)
Rhegmatogenous
- Varies by situation and surgeon
- Vitrectomy is the most commonly used procedure
- Scleral buckling can be used if there is no evidence of PVD
- Pneumatic retinopexy is used in cases of small tears between 11-1 clock hours
Tractional
- Vitrectomy with membrane peel
Exudative
- Aim to treat the underlying cause
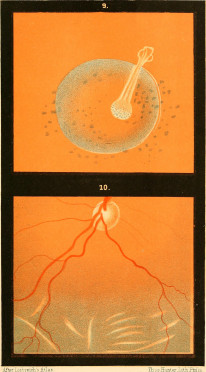
Posterior Vitreous Detachment
Separation of the posterior vitreous cortex from the internal retinal membrane.
Pathology
Liquefaction of the vitreous gel occurs with age → liquid seeps outside of the gel-matrix of the body of the vitreous → liquid accumulates between the outer membrane of the vitreous (vitreous cortex) and the internal limiting membrane of the retina.
- This process is known as syneresis and eventually leads to the detachment of the vitreous from the retina
- This process can also lead to tearing of the retina and associated vessels, leading to vitreous haemorrhage
If a retinal tear has occurred, pigmented retinal particles described as 'tobacco dust' can be seen in the vitreous. This is known as Shaffer sign.
Diagnostics
- Patients typically present in old age with flashing lights and floaters in their vision
- Visual acuity tends to be preserved
- Weiss ring can be seen
It is vitally important to look for tears because this dramatically increases the risk of RD. Associated retinal tears are treated with retinopexy (either laser or cryo).
Management
- PVD in itself does not require management other than vigilance for RD and its associated symptoms
- If the symptoms worsen or a visual field defect develops, they should immediately be investigated for RD
Vitreous Haemorrhage
Bleeding into the vitreous cavity.
Pathology
- Bleeding is either caused by traumatic injury or leakage during neovascular processes such as retinal vessel occlusion and DR
Diagnostics
- Vision is obstructed by blood, easily seen on fundoscopy
- Full fundus examination is needed to look for retinal damage
- B-scan can be used to evaluate the retina if the haemorrhage is extensive
Management
- Fundal view present → PRP
- Obstructed fundal view → Intravitreal anti-VEGF
- Persistent haemorrhage or associated RD → Pars plana vitrectomy
Hereditary Vitreoretinal Degenerations
Rare disorders are to be suspected in young patients who present with retinal/vitreous degenerations.
X-linked Retinoschisis
- A genetic disorder characterised by abnormally weak adhesions between layers of the retina. This leads to the splitting of the retinal layers
- Often affects the nerve fibre layer
- Typical presentation involves a young hyperopic boy with reading difficulties
- Examination will reveal bilateral maculopathy resembling CMO but no leakage on FFA
- Scotopic ERG will reveal a loss of the B wave
Retinal detachment must be distinguished from retinoschisis. There are various clinical differentiators for this, and the exam is likely to compare these.
Retinal Detachment |
Retinoschisis |
|---|---|
Relative scotoma |
Absolute scotoma |
Myopes higher risk |
Hyperopes higher risk |
Superotemporal |
Inferotemporal |
Corrugated surface |
Smooth surface |
No reaction to PRP |
Reaction to PRP |
Stickler Syndrome
- An AD disorder of type 2 collagen synthesis resulting in multiple systemic abnormalities including: deafness, marfanoid features, micrognathia and cleft palate
- Ocular manifestations include: cataracts, ectopia lentis, glaucoma, RRD and empty vitreous
- Patients are treated prophylactically with a retinal laser
Wagner Syndrome
- Similar to Stickler but no systemic associations
- Risk of RRD is much lower
Other Vitreoretinal Disorders
There are lots of other variations of vitreoretinal diseases. The important ones are summarised in this section.
Description |
Presentation |
Maangement |
|
|---|---|---|---|
Epiretinal Membrane |
An avascular membrane develops over the surface of the retina and can be visualised on fundoscopy |
Patients are typically asymptomatic |
Symptomatic cases can be treated with Vitrectomy |
Macular Hole |
A hole within the macula, extending the full-thickness of the neurosensory retina.. Can be primary, due to PVD where there is vitreomacular traction Can by secondary in causes unassociated with PVD such has trauma |
Central loss of vision and metamorphopsia |
Vitrectomy + internal limiting membrane peel + gas tamponade Ocriplasmin is a recombinant protease enzyme that can be used in macular holes caused by vitreomacular traction. |
Choroidal Detachment |
Abnormal accumulation of fluid between the choroid and sclera (suprachoroidal space) |
Typically seen in situations of acute hypotony such as the aftermath of glaucoma surgery. |
Often self-limiting. |
Uveal Effusion Syndrome |
Bilateral dysfunction of the choroid and ciliary body leads to ERD and choroidal detachment. |
Seen in middle-aged hyperopic men with nanophthalmos. |
Sclerotomy |


