Pupillary Reflexes
These pathways can be difficult to learn but it is worth having an idea of how these reflexes work. Once you understand these principles, you will be able to work out a lot of neurological problems.
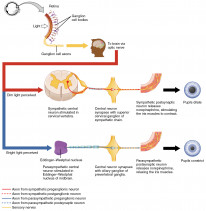
Miosis

Miosis is the constriction of the pupil:
- It is triggered by 2 key stimuli: light and near convergence.
- Each trigger has a separate pathway which leads to the activation of neurons in the Edinger-Westphal nucleus.
- The neurons lead to a parasympathetic response causing constriction of the sphincter pupillae muscle of the iris.
Afferent Limbs
- Pupillary light reflex (miosis in response to light)
- Retinal ganglion cells → optic nerve → chiasm → exit at optic tract before the lateral geniculate nucleus (LGN) → enter dorsal midbrain → synapse with ipsilateral pretectal nucleus → projections to bilateral Edinger-Westphal nuclei
- Near reflex (accommodation) (miosis, lens thickening and eye convergence)
- Visual cortex / CN3 → Frontal lobe eye fields → CN3/Edinger-Westphal nucleus
- CN3 → Medial recti → Convergence
- Edinger-Westphal nuclei → Pupil constriction and lens thickening
- Visual cortex / CN3 → Frontal lobe eye fields → CN3/Edinger-Westphal nucleus
Efferent Limb
The action of miosis is brought about by a single common pathway involving CN3:
- Edinger-Westphal nuclei → CN3 → Ciliary ganglion → Short ciliary nerves → Sphincter pupillae and ciliary body:
- Sphincter pupillae → miosis.
- Ciliary body → contraction of ciliary muscle → zonular relaxation → lens thickens (accommodation).
Defective mydriasis can lead to miosis and vice versa.
Mydriasis
Mydriasis is the dilation of the pupil
- It is a sympathetic response brought about by contraction of the dilator pupillae muscle of the iris.
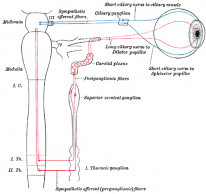
Pathway for Pupillary Dilation
The efferent limb of this reflex pathway follows the general route of sympathetic innervation to the head and neck, a 3-order system:
- First order fibres start in the hypothalamus and project down the spinal cord to C8-T10 (ciliospinal centre of Budge).
- Second order preganglionic fibres leave the spinal cord, traverse over the lung apex and synapse at the superior cervical ganglion at the carotid bifurcation.
- Third order post-ganglionic fibres traverse the wall of the internal carotid artery and enter the globe via long ciliary nerves to innervate the dilator pupillae.
The broad sympathetic pathway to the eye is: Hypothalamus → T1 → Superior cervical ganglion → ICA → long ciliary nerve → dilator pupillae. This sympathetic pathway is compromised in Horner syndrome.
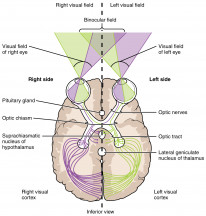
Visual Pathway
Starts in the retina and projects into the occipital cortex. Lesions after the retina typically result in hemianopia and quadrantanopia. Lesions of the retina tend to result in scotomas and are discussed in the next section.
The optic nerve (CN2)
Axons of the retinal ganglion cells wrap together to form the optic nerve.
Divisions:
- Intraocular: shortest and ends at the lamina cribrosa.
- Intra-orbital: longest and ends at optic foramen.
- Intracanalicular: through the optic canal into the middle cranial fossa.
- Intracranial: ends at the chiasm.
Blood supply:
- Intraocular → short posterior ciliary artery.
- Rest → ophthalmic artery (Pial vessels).
Chiasm
The axons travelling from the nasal part of the retina leave the optic nerve and decussate at the chiasm. The chiasm sits anterior to the hypothalamus and superior to the pituitary gland.
Willebrand's knee:
- It is an anterior notch of the optic chiasm where crossing inferonasal fibres of the optic nerve notch forward into the contralateral optic nerve before proceeding posteriorly to the contralateral optic tract.
- Pathology of this notch gives rise to junctional scotomas. I.e. Left-sided lesion of Willebrand's knee such as a tuberculum sellae meningioma, will result in loss of right superotemporal field and left blind eye (junctional scotoma).
Middle Chiasmal Lesions:
- Lesions affecting the body of the chiasm result in bitemporal hemianopia.
- Lesions from elsewhere can expand and compress the chiasm causing pathology:
- Pituitary adenomas compress the chiasm from below and cause bitemporal superior quadrantanopia progressing to bitemporal hemianopia.
- Craniopharyngiomas compress the chiasm from above and cause bitemporal inferior quadrantanopia progressing to bitemporal hemianopia.
- Middle lesions affecting the uncrossed temporal fibres are rare but can result in binasal hemianopia.
Posterior Chiasmal Lesions:
- The macular fibres cross posteriorly so posterior chiasmal lesions lead to paracentral scotoma.
The reason that lesions of the chiasm result in field loss that is opposite to the site of the lesion can be difficult to grasp at first. Remember that the lower part of the retina is responsible for the upper part of the visual field, and the upper part of the retina sees the lower visual field. I.e. In the case of a superior chiasmal lesion, the superior retinal ganglion fibres are damaged. This means the patient cannot see their lower field of vision. The lower visual field is seen by the upper retinal cells.
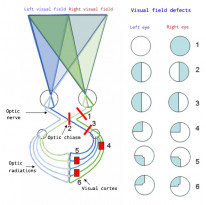
Optic Tract
There are 2 optic tracts, one for each hemisphere:
- They project from the chiasm to the LGN.
- They carry ipsilateral temporal axons and contralateral nasal axons.
- Lesions of the tract result in contralateral incongruous (asymmetrical) homonymous hemianopia. I.e. lesion of the right tract will result in left homonymous hemianopia.
- Lesions of the tract can also produce contralateral afferent RAPD because over half the fibres have already crossed at the chiasm.
Optic Radiations

Projections from the LGN to the visual cortex. The radiations are divided into superior (dorsal loop) and inferior (Meyer's loop) projections.
Dorsal Loop:
- The superior projection.
- It travels through the parietal lobe carrying inferior visual fields to the primary visual cortex, superior to the calcarine sulcus.
- E.g. Lesion of the left parietal lobe results in right inferior homonymous quadrantanopia.
Meyer's Loop:
- Meyer's loop is the inferior projection.
- It travels through the temporal lobe carrying superior visual fields to the primary visual cortex, inferior to the calcarine sulcus.
- E.g. Lesion of the left temporal lobe results in right superior homonymous quadrantanopia.
The dorsal loop has been mistakenly referred to as Baum’s loop in textbooks and journal articles. This was due to a false attribution on a Wikipedia article. More here: https://link.springer.com/article/10.1007%2Fs00276-020-02587-4
Occipital Cortex
The occipital cortex is where cognitive visual perception occurs. The exact mechanisms that underpin the conscious perception of vision are not known.
Lesions:
- Systemic hypoperfusion or back of head injury → homonymous hemianopia with central scotoma.
- Posterior cerebral artery occlusion → homonymous hemianopia with macular sparing (central vision spared).
Visual Streams
After the occipital cortex, there are 2 streams of neurons which project to 2 different cortical areas. The visual streams are responsible for a particular type of visual perception:
- The dorsal stream projects to the parietal lobe and is responsible for localising vision.
- The ventral stream projects to the temporal lobe and is responsible for visual identification.
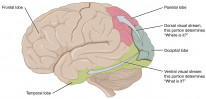
Visual streams. By OpenStax College, CC BY 3.0.
Scotomas and Visual Field Testing
The visual field extends approximately 50° superiorly, 60° nasally, 70° inferiorly, and 90° temporally. Perimetry is the clinical measurement of the visual fields.

Types of Field Loss
- Scotoma: Area of visual loss surrounded by normal visual area.
- Absolute scotoma: No light seen at all.
- Relative scotoma: Brighter lights are seen.
- Homonymous: Same visual field quadrants are affected in both eyes.
- Hemianopia: 2 quadrants of vision loss.
- Quadrantanopia: 1 quadrant vision loss.
- Congruousness: the degree to which the defects are the same in both eyes, increases as you move posteriorly in the tract.
- Seidel scotoma: enlargement of blind spot.
Bear in mind that the ipsilateral axons correspond to the contralateral fields. A good way to think about this is to differentiate the visual field from the retinal axon area. I.e. the temporal axons correspond to the nasal visual field.
Perimetry


Perimetry is the measurement of visual fields.
Humphrey:
- Humphrey visual field analysis is automated and static.
- This test is conducted by a computer where stationary stimuli are presented at specific locations of the visual field.
Goldmann:
- Goldmann visual field testing is manual and kinetic (a stimulus is moved towards the centre, from the edge of the visual field).
- Manual testing requires an examiner to conduct the assessment.
Esterman:
- Esterman visual field testing is binocular and used by the DVLA to assess driving aptitude.
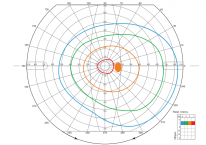
Goldmann visual field record sheet. By Юкатан, CC BY-SA 4.0 .
There are many tests that are used to measure the visual fields. The high-yield ones are outlined above.
Colour loss
Certain diseases are characteristically associated with specific types of colour blindness.
Red-Green loss
- Optic nerve problems such as neuritis.
- Except glaucoma!
Blue-Yellow loss
- Macular problems such as AMD.
- And glaucoma!
Extraocular Muscles
Eye movements are produced by 6 ocular muscles: 4 recti and 2 obliques.
- MR → medial rectus
- LR → lateral rectus
- SR → superior rectus
- IR → inferior rectus
- SO → superior oblique
- IO → inferior oblique

Extraocular muscle anatomy By OpenStax College, CC BY 3.
Functional Descriptions
- Antagonist-agonist: muscles in the same eye that move in opposite directions i.e. right MR and right LR.
- Sherrington's law: Increased innervation of an agonist results in a decreased innervation of its antagonist.
- Synergists: muscles in the same eye that move in same direction i.e. right SO and right IR.
- Yoke muscle: muscle in the opposite eye which moves both eyes in the same direction i.e. left LR and right MR.
- Hering's law: yoke muscles receive equal innervation. I.e. contraction of left LR will simultaneously produce equal contraction of the right MR.
Origins
- All recti originate from the common tendinous ring (Annulus of Zinn).
- SO originates from the lesser wing of sphenoid.
- IO originates from the orbital floor.
Medial rectus inserts closest to the limbus and superior rectus inserts furthest away.
Innervation
- CN6 → LR
- CN3 → All other recti + IO
- CN4 → SO
Actions
- Elevation → SR (Primary) + IO
- Depression → IR (Primary) + SO
- Adduction → MR (Primary) + SR + IR
- Abduction → LR (Primary) + SO + IO
- Intorsion → SO
- Extorsion → IO
Cranial Nerves 3,4,6
The oculomotor nerve (CN3), the trochlear nerve (CN4) and the abducens nerve (CN6) are all involved in the innervation of the extraocular muscles.
Nucleus locations
- CN3 → dorsal midbrain at the level of the superior colliculus.
- CN4 → dorsal midbrain at the level of the inferior colliculus.
- CN6 → ventral to 4th ventricle at pontine tegmentum near the paramedian pontine reticular formation.
Pathways



CN3 Pathway
- Origin at the level of the superior colliculus in the dorsal midbrain.
- Exits brainstem anteriorly through the interpeduncular fossa.
- Passes between posterior cerebral and superior cerebellar arteries.
- Travels through the lateral wall of cavernous sinus superior to CN4.
- Bifurcates into a superior and inferior branch.
- Enters orbit through the SOF within annulus of Zinn.
CN4 pathway
- Origin at the level of the inferior colliculus in the dorsal midbrain.
- Exits brainstem dorsally and decussates.
- Passes between posterior cerebral and superior cerebellar arteries.
- Travels in lateral wall of the cavernous sinus.
- Enters orbit through SOF above the annulus of Zinn.
CN6 pathway
- Origin at pontine tegmentum, ventral to the 4th ventricle.
- Exits brainstem anteriorly at the pontomedullary junction.
- Traverses Dorello's canal near the petrous part of the temporal bone (susceptible to stretching by increased pressure).
- Travels within the cavernous sinus, lateral to the ICA.
- Enters orbit through SOF within the annulus of Zinn.

Anatomy of the cranial nerves at the cavernous sinus. Note how only CN6 travels within the sinus whereas the rest of the nerves travel within the wall of the sinus. By Okkes Kuybu, MD, CC BY 4.0.
CN4 is most likely to be damaged by trauma because it has the longest course. CN6 is most likely to be damaged by raised ICP because it travels within Dorello's canal where it is tightly packed against hard bony structures.
Actions
CN3
- Ipsilateral IO IR MR.
- Contralateral SR.
- Bilateral levator.
- Ipsilateral sphincter pupillae.
CN4
- Contralateral SO.
CN6
- Ipsilateral LR.
Gaze
Your gaze is controlled at 3 levels: supranuclear (initiates movement at the cortex), intra-nuclear (coordinates movement at the brainstem), and infra-nuclear (efferent nerves to muscles). There are also 3 important types of gaze you should be aware of: saccades, smooth pursuit and vestibular ocular movements.
Saccades
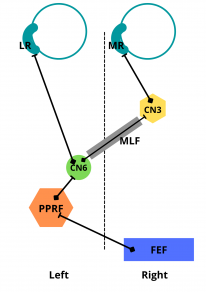
Rapid movements to fixate on objects
- Voluntary saccades are initiated in the frontal lobe, contralateral to the direction of horizontal movement.
- For example, a right saccade is initiated at the left frontal cortex.
Horizontal Saccade Pathway
Frontal lobe frontal eye field (FEF) → Pons → Pontine paramedian reticular formation (PPRF) → CN6 → Medial longitudinal fasciculus (MLF) → Contralateral CN3
- Impulse originates from the frontal lobe on the contralateral side to the intended direction of Gaze. For example, an attempt to initiate a gaze to the RIGHT originates in the LEFT frontal lobe. This is the supranuclear origin of action.
- Impulse reaches the pons.
- At the pons it activates the PPRF and CN6 nucleus. At this point, the impulse splits into 2 pathways:
- One pathway advances down CN6 and acts on the ipsilateral lateral rectus muscle → abduction.
- Another pathway connects the CN6 nucleus to the contralateral CN3 nucleus. From the CN3 nucleus, it acts directly on the corresponding medial rectus → adduction.
I.e. When someone looks LEFT: RIGHT frontal lobe → LEFT PPRF → LEFT CN6 nucleus (LEFT lateral rectus) → RIGHT MLF → RIGHT CN3 nucleus (RIGHT medial rectus).
The horizontal gaze pathway can be tricky to grasp at first but is well worth learning because it is frequently tested. Abnormalities in this pathway are discussed in the gaze abnormalities section.
Smooth pursuit
Slow tracking of moving objects
- Initiated by the Parietal-occipital-temporal (POT) region, ipsilateral to the tracking direction.
- For example, right slow pursuit is initiated by the right POT.
Vestibular ocular movements
Keep eyes stable with head movement
- Initiated at brainstem level, does not involve the cortex.
Tested by doll's head reflex:
- The eyes move when the head is moved to keep them looking in the same direction.
- If the doll's head reflex is intact, then the internuclear pathways must be intact.
Nystagmus
Nystagmus is repeated, involuntary oscillation of the eyes. It can be physiological or pathological.
Physiological
- Occurs at extremes of gaze or by following fast-moving objects.
Pathological
- Upbeat → medullary lesions.
- Downbeat → Arnold-Chiari malformation.
- Vestibular → vestibular lesion causes nystagmus towards the lesion.
- Latent → horizontal nystagmus that starts when one eye is covered. Beats towards the covered eye. Associated with infantile esotropia.
- Convergence retraction nystagmus → bilateral convergence and retraction of the globe on attempted upgaze.
Congenital nystagmus can be caused by bilateral cataracts and neurological disorders.


