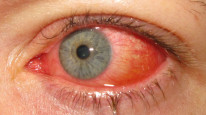
Inflammation of the conjunctiva is most commonly due to an acute, self-limiting viral infection. Be vigilant and escalate cases with corneal involvement (keratitis).
Overview
Follicles vs papillae
Conjunctivitis has 2 distinct clinical appearances which help you differentiate the potential causes.
Papillae
- Papillae have a red (blood vessel) center and flat top.
- More common on the upper lid.
- Associated with: allergic, bacterial & toxic conjunctivitis.
Follicles
- Dome-shaped discrete transparent lesions.
- More common on the lower lid.
- Associated with: viral & chlamydial conjunctivitis.
Broad Presentations
Bacterial |
Acute/hyperacute red sticky eyes with purulent discharge |
|---|---|
Viral |
Acute red watery eyes with lymphadenopathy |
Chlamydial |
Subacute unilateral red eyes with persisting mucopurulent discharge and lymphadenopathy |
Gonococcal |
Hyperacute (<24hrs) red eyes, keratitis, and severe purulent discharge with STI risk factors |
Allergic |
Acute/recurrent red itchy eyes with watery discharge |
General management
- Conjunctival swabs for microbial investigations are reserved for severe/atypical cases and not routinely indicated in simple acute bacterial/viral conjunctivitis.
- Specific treatment depends on the type of conjunctivitis (see sections below).
Bacterial Conjunctivitis
Bacterial infection of the conjunctiva is common, often self-limiting, and frequently encountered in primary care. It should be suspected in patients with red gritty sticky eyes and purulent discharge.
Pathology
Causes
- Cool climates → Streptococcus pneumoniae and Haemophilus influenzae.
- Warm climates → Haemophilus aegyptius.
- Children → Haemophilus influenzae.
Chronic Pathology
- Chronic and relapsing conjunctivitis typically indicates the presence of a nearby reservoir colony.
- This should be suspected in the case of chronic dacryocystitis, staph blepharitis and giant fornix syndrome.
Giant fornix syndrome is characterised by the sequestration of bacteria in the upper fornix of the conjunctiva and is typically seen in the elderly.
Diagnostics

Presentation
- Acute/hyperacute red sticky eyes with purulent discharge.
- Typically bilateral but often starts unilaterally.
- Patients complain of their eyes being stuck together in the morning.
Investigations
- Diagnosis is clinical.
- Conjunctival swabs for microbiology are only required in unresolving cases or severe infections.
Any involvement of the cornea (keratitis) can be sight-threatening and warrants admission for further workup.
Management
Initial
- Practice good hand and eye hygiene.
- Advise the patient to return if the infection doesn't self-resolve within a week or gets worse.
- Switch to spectacles from contact lenses during the episode.
Medications
- Topical chloramphenicol drops.
- Systemic antibiotics are reserved for gonococcal conjunctivitis in adults or H. influenzae/Meningococcal conjunctivitis in children.
- H. influenzae → PO Co-amoxiclav.
Chloramphenicol is associated with aplastic anaemia, though the risk is extremely small with topical use.
Adult Inclusion Body Chlamydial Conjunctivitis
Chlamydia trachomatis can cause 2 different types of conjunctivitis and it's important to be aware of both types: trachoma and inclusion body. This section will discuss inclusion body.
Pathology
- Caused by Chlamydia trachomatis, a gram-negative intracellular obligate bacterium.
- Associated with serotypes D-K of Chlamydia trachomatis.
Serotypes L1, L2, L3 cause Lymphogranuloma Venereum.
Diagnostics

Presentation
- Subacute (2-3wks) unilateral conjunctivitis in young people.
- Associated with STI symptoms such as urethritis.
- Inferior follicular conjunctivitis with persisting mucopurulent discharge and lymphadenopathy.
Investigations
- Conjunctival swab for PCR provides prompt diagnosis.
Giemsa stain shows basophilic intracytoplasmic inclusion bodies.
Management
- 1g oral azithromycin STAT or 100mg doxycycline BD for 14 days.
Trachoma
Trachoma is a highly infectious epidemic conjunctivitis seen in developing countries. It is the leading cause of preventable blindness worldwide.
Pathology
- Caused by Chlamydia trachomatis serotypes A-C.
- Acute conjunctivitis is caused by the pore-like infectious particle (elementary body) of chlamydia.
- A type 4 hypersensitivity reaction occurs after initial infection → scarring → trichiasis and entropion → corneal damage → blindness.
The conjunctival scarring leads to entropion, where the lids roll inwards. This causes the lashes to rub against the cornea when blinking.
Presentation
- Seen in poverty and crowded places.
- Chronic superior follicular conjunctivitis.
- Herbert pits (depressions of superior limbus).
- Arlt's line (a thick band of scar tissue in the conjunctiva).
- Trichiasis and entropion.
Management
WHO SAFE strategy:
- Surgery for trichiasis (bilamellar rotation).
- Azithromycin 1g PO.
- Facial hygiene.
- Environmental improvement.
Adult Gonococcal Conjunctivitis
Gonococcal conjunctivitis is approached differently in children vs adults. This section will cover adult gonococcal conjunctivitis.
Pathology
- Caused by infection with Neisseria gonorrhoeae, a gram negative diplococcus.
- These patients can be severely unwell.
Diagnostics
Presentation
- Hyperacute and with severe pain, tearing and red-eye.
- Conjunctival membranes and preauricular lymphadenopathy.
Investigations
- Conjunctival swab for microbiology and referral to GUM clinic for sexual health follow-up.
Management
- Treat all with topical fluoroquinolone drops (ofloxacin or ciprofloxacin).
- Ceftriaxone IM 1g STAT to treat gonorrhoea.
- If keratitis → admit for IV ceftriaxone.
Ophthalmia Neonatorum
Conjunctivitis within the first 28 days of life
Cause |
Treatment |
Notes |
|---|---|---|
Chlamydia |
PO erythromycin |
Most common cause. Can progress to chlamydial pneumonitis |
Gonococcal |
IM ceftriaxone and IV penicillin |
Typically presents within the first 3 days of birth |
HSV |
IV acyclovir |
Presents with watery discharge and vesicular rash |
Staphylococcus |
Topical chloramphenicol |