Glaucoma is defined as: progressive optic neuropathy with characteristic changes in the optic disc and corresponding loss of visual fields (VF). It is the second leading cause of blindness worldwide.
It is the final common pathway for several conditions associated with raised intraocular pressure (IOP). It can be considered as an umbrella term for these conditions.
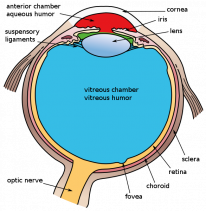
Aqueous humour (AQH)
Glaucoma is caused by a disorder in the normal flow of aqueous humour. It is important to understand aqueous humour in detail.
Physiology
Aqueous humour supplies nutrients to the cornea and lens:
- It flows from the posterior chamber to the anterior chamber via the pupil.
- It fills the anterior chamber at 0.25mL (larger than the posterior chamber).
- It is composed of 99% water and has a lower glucose and protein concentration than plasma.
Production and secretion
Aqueous humour is formed by the non-pigmented inner epithelium of the ciliary processes at the pars plicata:
- The inner non-pigmented epithelium is continuous with the neural retina.
- Most secretion occurs by active transport which is under sympathetic control:
- Stimulation of beta-2 receptors increases secretion.
- Stimulation of alpha-2 receptors decreases secretion.
The ciliary body also has an outer pigmented epithelium that is posteriorly continuous with RPE.
Drainage
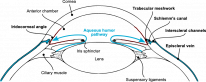
AQH travels from the posterior chamber to the anterior chamber via the pupil (the hole in the iris centre). There are 2 main pathways for AQH to drain from the eye:
Trabecular path (90%)
- Also known as the conventional route.
- AQH flows through the trabecular meshwork → Schlemm's canal → episcleral veins.
- Contraction of ciliary muscle increases trabecular outflow.
Uveoscleral path
- AQH passes directly outward through ciliary muscle → suprachoroidal space → choroidal veins → vortex veins.
Trabecular Meshwork (TM)
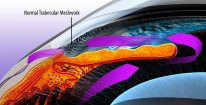
The TM is a band of cellular sheets which form a sieve-like structure. It is triangular in cross-section and is found at the anterior chamber angle.
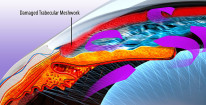
It consists of 3 parts:
- Innermost → uveal meshwork with large holes.
- Middle → corneoscleral meshwork with smaller holes.
- Outermost → juxtacanalicular meshwork connects TM to Schlemm canal.
The juxtacanalicular meshwork contains the narrowest spaces and confers the largest resistance to normal AQH outflow via the conventional route.
Scleral Spur
A fibrous projection from the sclera.
- Longitudinal ciliary muscles insert onto its posterior surface.
- It is an important landmark in gonioscopy.
Anterior Chamber (AC) Angle
- Extends from Schwalbe's line (termination of Descemet's membrane of the cornea) to the TM, scleral spur and ciliary body.
- Clinically significant because the closure of the angle will impede AQH outflow via the conventional route.
Angle-closure → AQH outflow blocked → AQH buildup → increased IOP → optic neuropathy → visual field defects → angle-closure glaucoma.
Assessment of Glaucoma
Diagnosis is based on the 'glaucoma triad': raised IOP, abnormal disc, and visual field defects. The latter 2 signs are most important.
Intraocular Pressure
Goldmann tonometry is the gold standard method of measuring intraocular pressure:
-
Normal range is 11-21 mmHg.
-
Diurnal variation of up to 5 mmHg is normal. Peaks in the morning.
-
Supine positioning leads to higher IOP than sitting.
-
IOP measurement is affected by corneal thickness, astigmatism and the axial length of the eyeball.
You do not need raised IOP to diagnose glaucoma!
Optic Disc Changes
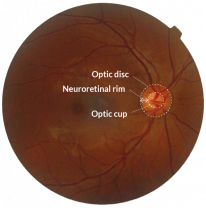

Glaucomatous disease processes invariably damage the optic nerve; evidence of this damage can be seen in the optic disc during fundoscopy:
- The neuroretinal rim is the border of the optic disc and contains the retinal neuronal cells. The centre of the disc is the cup and contains the central retinal vessels.
- Neuroretinal rim thickness follows the ISNT rule of thickness: inferior (thickest), superior, nasal and temporal (thinnest).
- In glaucoma, the neuroretinal rim becomes thinner so that it no longer follows the order of the ISNT rule. This is called cupping of the disc.
- A normal cup-to-disc ratio is around 0.3.
- In glaucoma, the cup-to-disc ratio is increased.
- Nasal vessel displacement and haemorrhages at the disc are also signs of glaucomatous change.
Decreased nerve fibre layer (NFL) thickness readings on OCT would make one suspicious for optic nerve damage.
Visual Fields

Perimetry is the measurement of visual field defects:
- The best test for monitoring glaucoma is Humphrey 24-2 perimetry.
- Glaucomatous visual field defects occur as a result of damage to the retinal nerve fibres.
Gonioscopy
Gonioscopy is a method of visualizing the anterior chamber angle, it is important in identifying angle-closure glaucoma. Peripheral anterior synechiae might be found in angle closure, this is the iris bowing forward and closing off the angle.

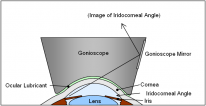
Order of structures seen on gonioscopy from superficial to deep:
- Posterior corneal surface
- Schwalbe's line
- Non-pigmented trabecular meshwork
- Pigmented trabecular meshwork
- Scleral spur
- Ciliary body
- Iris
- Pupil
Medical treatment
Glaucoma drugs are commonly tested in the exam. You should be aware of their mechanisms of action and side effects.
Medical treatment can on average lower IOP by 20-30% (5-7mm Hg).
Prescribing
Order of use:
- Latanoprost
- Timolol
- Brinzolamide
- Brimonidine
Except in pregnancy/paediatrics:
- No eye drops are licensed for children or pregnant women. Use brimonidine in the first trimester and switch to timolol in 3rd.
Compliance is almost always an issue when you prescribe more than 2 drops over time.
Drug class |
Mechanism of Action |
Side Effects |
Contraindications |
|---|---|---|---|
Prostaglandin agonists (e.g Latanoprost) |
|
|
|
Beta-Blockers (e.g Timolol) |
|
|
|
Alpha 2 agonists |
|
|
|
Cholinergic agonists (e.g Pilocarpine) |
|
|
|
Carbonic anhydrase inhibitors (e.g Brinzolamide (any -lamide)) |
|
|
|
Order of use: Prostaglandins > Beta-blockers > Alpha 2 agonists > Cholinergics > Carbonic anhydrase inhibitors
The major distribution of beta receptors is: 1 heart, 2 lungs, 3 adipose
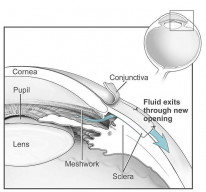
Trabeculectomy
Performed in chronic glaucoma where medications have failed to control IOP.
- The creation of a fistula from the anterior chamber to the sub-tenon space - creating a bleb (elevation of the conjunctiva where the aqueous gathers).
- Antimetabolites can be used adjunctively to slow the healing process and prevent bleb failure:
- 5-FU: pyrimidine analogue which inhibits fibroblasts by blocking DNA synthesis.
-
Mitomycin C: alkylating agent which inhibits fibroblasts.
Conventional Trabeculectom
Laser surgery
Procedure |
Indication |
Laser |
|---|---|---|
Peripheral iridoplasty - contraction burns of the peripheral iris pull it away from the angle |
Temporising measure in acute angle-closure |
Argon (455-529nm) |
Peripheral iridotomy - creates a hole in the peripheral iris to allow aqueous flow through a closed-angle |
Definitive treatment in acute angle-closure |
ND: YAG (1064nm) |
Selective laser trabeculoplasty (SLT) - laser applied to the trabecular meshwork to facilitate drainage |
Used in open-angle glaucoma where medical treatment is not tolerated |
Frequency-doubled Q-switched ND: YAG (532nm) |
Selective laser has replaced argon laser in trabeculoplasty.
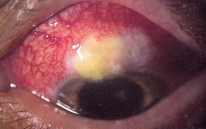
Iatrogenic Glaucoma
Raised IOP is not uncommon in the post-surgical patient. Cataract and vitreoretinal surgeries are the most associated and will be discussed in this section.
Post-Vitreoretinal Surgery
-
Intraocular gases can raise the IOP due to gas expansion.
- Usually, short-term acetazolamide is enough to control IOP but consider the half-life of the gas.
- Scleral buckling can cause secondary angle-closure due to ciliary body swelling, but this usually resolves spontaneously.
-
Silicone oil blocks the trabecular meshwork.
- Usually resolves spontaneously.
- Try cyclodestruction if it persists.
- Vitrectomy via ghost cell glaucoma (discussed further in the secondary open-angle glaucoma chapter).
Post-Cataract Surgery
- Usually due to retained viscoelastic, retained fragments or inflammation.