The eyelid plays a vital role in ocular surface health. It sweeps away debris and maintains the tear film. Without eyelids, the tear film would evaporate and give way to ulcerations of the ocular surface.
Any damage to the cornea can be sight-threatening.
Anatomy and Physiology
Structure
Eyelid tissue layers from anterior to posterior:
- Skin
- Orbicularis muscle
- Tarsal plate (fibrous)
- Levator muscle
- Muller muscle
Lamellae
- The eyelid is anatomically divided into 2 lamellae (sections) by the Gray line, the outermost margin of the Orbicularis muscle.
- Anterior lamella contains: skin and orbicularis.
- Posterior lamella contains: tarsal plate and conjunctiva.
Normally, the upper lid is 2mm below the superior limbus and the lower lid is at the level of the inferior limbus. This is important in disorders of lid position, where the lids will not be positioned as such.
Orbital Septum
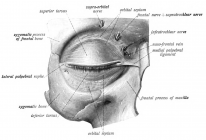
- The orbital septum is a fibrous sheet that originates from the fascia and periosteum of the orbital rim.
- As the septal sheet descends to the aperture between the upper and lower lids it becomes thicker and forms the tarsal plates.
- The tarsal plates maintain the shape of the eyelids.
- There is a layer of preaponeurotic fat pads just posterior to the orbital septum. This is useful in categorising the depth of lacerations. If the fat pads are visible then it is a deep laceration involving the posterior lamella.
The orbital septum is an important radiological landmark in the classification of orbital cellulitis (see orbital chapter).
Muscles of eyelid control
Eyelid Retraction
There are 3 muscles of retraction: levator palpebrae superioris (main), Müller's muscle and frontalis.
- The levator originates from the lesser wing of the sphenoid bone and inserts onto the anterior aspect of the tarsal plate, passing over the lateral rectus.
- The levator is innervated by CN3.
- Frontalis is a muscle of facial expression and is innervated by CN7 (facial nerve).
- Müller's muscle is under sympathetic innervation.
Eyelid Closure
- Orbicularis oculi is the main muscle of eyelid closure.
- It is innervated by CN7.
The orbicularis muscle also plays an important role in the lacrimal pump mechanism where its action guides the flow of tears across the ocular surface.
Blink Reflex
Afferent Limb (3 inputs paths)
- Corneal stimulus via CNV1.
- Light stimulus via CN2.
- Auditory stimulus via CN8.
Efferent limb (1 effector path)
- The efferent limb is via CN7 to the Orbicularis oculi muscle, which controls lid closure.
Bell's phenomenon
- Bell's phenomenon is a normal physiological finding where the globe rotates up and out during forced lid closure.
- A poor Bell's phenomenon is a risk factor for lagophthalmos.
Canthal tendons
- The canthal tendons keep the eyelid structure stable.
- There are 2 in each orbit: a medial and a lateral.
- They attach to the tarsus of the upper and lower eyelids.
The lacrimal sac lies between the limbs of the medial canthal tendon.
Palpebral Fissure Presentations
The palpebral fissure is the gap between the upper and lower eyelid margins. Abnormalities of the eyelid muscles can cause them to be abnormally retracted or droopy (ptosis). The table below summarises the key conditions for the exam.
Disease |
Presentation |
Mechanism |
|---|---|---|
Thyroid eye disease |
Retraction |
Müller contraction |
Horner syndrome |
Ptosis |
Müller relaxation |
CN7 palsy |
Lagophthalmos |
Orbicularis weakness |
CN3 palsy |
Ptosis |
Levator relaxation |
Lagophthalmos is the inability to fully close the eyelids (palpebral fissure). This leads to exposure keratopathy, which can be sight-threatening.
Lid Reconstruction (Oculoplastics)
Lid lacerations are not uncommon. It is important to note the depth of the laceration if both lamellae are involved. This is because different procedures are used on the different lamellae.
Types of reconstruction
Type |
Description |
|---|---|
Direct Closure |
Use of surrounding skin to close the excision |
Flaps |
Rotation of local skin to close the excision with intact blood supply |
Grafts |
Transplant of distant skin. The priority order of skin graft site is: Other lid → preauricular → post auricular → under arm |
You cannot repair both lamellae with grafts because there would be no blood supply.
Techniques
Anterior lamella
- Anterior advancement → incise and stretch tissue over the laceration.
- Transposition → move tissue from the other lid.
- Rotation → rotated skin from the cheek.
- Glabella → rotated diamond-shaped forehead skin.
Posterior lamella
- Hughes Flap → flap taken from the upper lid.
- Free tarsal graft from the fellow eye → tissue taken from the other eye.
After a full-thickness laceration of the lid, both the posterior and anterior lamellae will need reconstruction. The posterior lamella (tarsus and conjunctiva) is repaired before the anterior lamella (skin and orbicularis).

