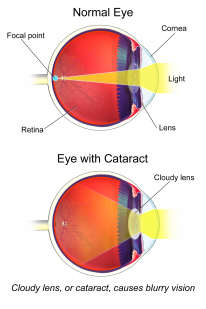
Cataract is the second commonest cause of vision impairment in the world. There is huge inequity in the global treatment of cataracts, with blindings cases only really being found in the developing world. This page will review the types of cataracts and discuss the relevant management procedures.
Overview
The exact pathomechanism is unknown but there are many types of cataracts and the diagnosis is readily made during clinical examination.
Pathology
- Alongside ageing, there is a decrease in the overall biochemical activities of the lens and a loss of antioxidants. This causes the lens to become thicker, weightier and cloudier, resulting in light scatter
- 2 types of crystallins are specifically affected with age:
- Alpha and gamma decrease
- Beta becomes more dispersed.
Grade
The extent of the cataract is categorised based on appearance:
- Immature - partially opaque
- Mature - opaque
- Hypermature - cataractous material is leaking outside the capsular bag and the capsule itself has shrunk, and wrinkling can be seen
- Morgagnian cataract - cortex has liquified and the nucleus has sunk within the capsular bag
Classification of Age-related Cataracts
Cataracts are often associated with age and the table below outlines the commonest types.
Type |
Key Features |
|---|---|
Nuclear sclerotic |
|
Cortical |
|
Anterior sub-capsular |
|
Posterior sub-capsular |
|
Classic Cataract Associations
There are several unique cataracts which are characteristically associated with certain diseases. These associations are summarised in the table below.
Cataract |
Disease |
|---|---|
Christmas tree cataract |
Myotonic dystrophy |
Blue dot cataract |
Down syndrome |
Pearly nuclear sclerotic cataract |
Rubella |
Sunflower cataract |
Wilson’s disease |
Shield cataract |
Atopic dermatitis |
Congenital Cataracts
- Most commonly occur bilaterally and follow an autosomal dominant inheritance pattern
- There are many secondary causes of congenital cataracts such as Down’s syndrome and homocystinuria. This list is extensive and unlikely to be worth learning in detail.
- The timing of surgery for congenital cataracts is based on balancing the risk of glaucoma and amblyopia
- Unilateral congenital cataracts should be removed at 6 weeks
- Bilateral congenital cataracts should be removed at around 10 weeks
Management
Cataract surgery is a core component of ophthalmic practice. The management plan has 3 principal components: assessment, intra-op and post-op. During the procedure, the cataractous lens is removed and a plastic lens is implanted in its place.

Biometry
Once a patient has been referred for cataract surgery, biometry is conducted to decide which type of lens implantation is best for the patient
- There are various machines that conduct biometry such as the IOLmaster
- Measurements include the axial length, corneal curvature and anterior chamber depth
- The numbers from these measurements are plugged into predictive formulae to find the appropriate power for the lens implant which will replace the cataract
Types of Lens Implants
-
These implants are called intraocular lenses (IOLs), don’t mistake this for the crystalline lens, which is the one you’re born with

An IOL implant. By: Frank C. Müller, CC BY-SA 3.0 via Wikimedia Commons -
There are 2 broad types of IOL: rigid and flexible
- Rigid is made of polymethylmethacrylate (PMMA) and is not widely used in the UK because it is associated with more complications, but it is cheap
- Flexible IOLs have 3 further subtypes
- Silicone - highest complication rates so not widely used in modern settings
- Acrylic hydrophobic - high refractive index but can cause glare
- Acrylic hydrophilic - best for biocompatibility
Consent
There are several important aspects of consent for cataract surgery
- 0.1% risk of sight-threatening complications such as endophthalmitis, retinal detachment and choroidal haemorrhage
- The commonest intra-op complication is posterior capsular rupture with vitreous loss - 4% risk
- The commonest post-op complications is posterior capsular opacification, 10% risk in 2 years
Techniques
- Phacoemulsification surgery is considered the gold standard and is widely practised. It uses ultrasound and suction to break the cataract into small fragments and to remove it from the capsular bag.
- Extracapsular cataract extraction (ECCE) is a manual operative method which has been superseded by phacoemulsification. It requires a larger incision, resulting in longer recovery and a higher risk for complications.
ECCE may still be used if the cataract is extremely hard and the surgeon is unable to break it with ultrasound.
Phacoemulsification Procedure
- Generic preparations with antiseptic, appropriate anaesthesia (typically topical or sub-Tenon's) and mydriasis
- Cleaning the external ocular structures with 5% povidone-iodine (is the most important step in preventing endophthalmitis)
- 1 main incision and 1/2 side ports created on the sclera using a blade or femtosecond laser
- Capsulorhexis - creation of a continuous curvilinear opening in the anterior capsular bag
- Hydrodissection - saline solution injected between the capsule and cortex to allow rotation
- Phacoemulsification - cataract broken with direct contact of the ultrasound tip on the nucleus and fragments aspirated
- IOL insertion - Fill bag with viscoelastic gel and inject IOL
- Remove viscoelastic gel
- Inject intracameral cefuroxime - another important step in preventing endophthalmitis
The femtosecond laser is an automated method of creating reproducible incisions
The ultrasound tip is called the phaco tip and it vibrates at 40-45kHz
Intraoperative Complications
There are 4 main intraoperative complications which occur during cataract surgery: posterior capsular rupture, zonular dehiscence dropped nucleus and choroidal haemorrhage.
Vitreous loss can also occur alongside these complications. The vitreous is encapsulated by the hyaloid membrane and vitreous loss occurs when this membrane is damaged and vitreous humour leaks. In these cases, the vitreous material is stained with triamcinolone and a vitrectomy is performed
Posterior Capsular Rupture
- Every effort is made to keep the capsular bag intact, so the IOL can be inserted.
- The posterior lens capsule is thinner than the anterior and is prone to rupture
- Typical signs include: sudden deepening of the anterior chamber and momentary pupillary dilation
- If there is a large rupture then it may not be possible to place the IOL implant within the capsular bag. In which case it can be placed anteriorly in the sulcus.
Posterior capsular rupture with vitreous loss is the most common intraoperative complication
Zonular Dehiscence
- Damage to the zonular fibres can make the lens unstable and complicate the surgical procedure
- Iris hooks can be used to secure the affected area and a capsular tension ring can be used to stabilize the lens capsule for the remainder of the procedure
Floppy iris syndrome is when the iris is flaccid. This complicates surgery because it gets in the way of the operation and isn’t fixed into position. It is classically associated with alpha-blockers such as tamsulosin (a drug used in the management of prostatic hyperplasia)
Dropped Nucleus
- This is when lens nucleus fragments escape the capsular bag. This material is inflammatory
- Small fragments can be addressed with post-operative steroids
- Large fragments may need removal via vitrectomy
Choroidal Haemorrhage
- Bleeding from the choroid is a serious sight-threatening complication with a 0.1% risk of occurrence during surgery
- Typical signs include: suddenly elevated intraocular pressure, shallowed anterior chamber, darkening/loss of the red reflex and severe pain
- Management involves the immediate suturing all of wounds + IV acetazolamide/mannitol + topical steroids
Choroidal haemorrhage is the ophthalmologist's worst nightmare. The prognosis is poor and most patients end up with severe visual impairment
Postoperative Complications
Post-op complications are classified as early (within days) or late. There are several notable conditions which are reviewed in this section.
Early
Corneal oedema is most common and is managed with topical steroids/NSAIDs. Return to the theatre if there is wound leakage or iris prolapse
Endophthalmitis
-
0.1% risk after cataract surgery

The white fluid line at 6’o clock is a hypopyon. By: Rakesh Ahuja, M.D. CC BY-SA 2.5 -
Sight threatening and required immediate treatment
-
Typically occurs within the week of surgery
-
Presents with pain, worsening vision and hypopyon (pus in the anterior chamber)
-
Anterior chamber tap and vitreous biopsy are used for diagnosis and microbiology
-
Treatment is with intravitreal vancomycin + Ceftazidime or Amikacin
-
Biopsy and antibiotics are administered simultaneously and can be repeated if there is a poor response
-
Severe cases with very low visual acuity are treated with pars plana vitrectomy
The most important step to prevent endophthalmitis is to clean the external ocular structures with povidone iodine before the surgery. Infective agents are often transmitted from the patients' own skin.
Late
Cystoid Macular Oedema (CMO) (Irvine-Gass syndrome)
- Tractional stress of surgery leads to the release of inflammatory mediators that cause oedematous fluid accumulation in perifoveal vessels around the macula
- Typically occurs within weeks of surgery
- Presents with painless blurry vision
- Diagnosis is made with OCT
- Management is targeted at mitigating the inflammatory process
- Starting with steroid drops
- 2nd step to periocular triamcinolone
- 3rd step to intraocular steroids
- If medications fail then vitrectomy might prove useful
Posterior Capsular Opacification (PCO)
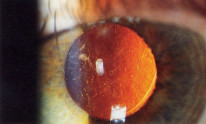
- 10% risk within 2 years
- Typically manifests as blurry vision some months after surgery
- Treatment with Nd: YAG laser capsulotomy

