The retina is essentially the cup at the end of CN2. Retinal cells are highly vulnerable to ischaemia and other vasculopathies.
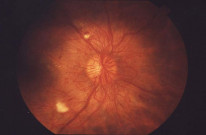
Diabetic Retinopathy
Diabetic retinopathy is the most common microvascular complication of diabetes mellitus. The cause of visual impairment in patients with diabetic retinopathy is often due to diabetic macular oedema.
Pathology
The fundamental pathomechanism is: Hyperglycaemia → damage to endothelial wall and pericytes.
This process has several important effects:
- Pericyte damage → microaneurysms → flame haemorrhages (nerve fibre layer).
- Infarcts → cotton wool spots (axonal debris at infarct margins) (nerve fibre layer).
- Increased vessel permeability → Hard exudates (lipoproteins in outer plexiform layer).
- Cystoid macular oedema (outer plexiform layer).
- Neovascularisation.
The most important risk factor for the progression of diabetic retinopathy is the duration of diabetes.
Presentation
Most cases are picked up with diabetic screening but there are 3 associated presentations to be aware of:
- Acute painful vision loss: Neovascular Glaucoma.
- Flashes/Floaters then painless vision loss: Vitreous haemorrhage or retinal detachment.
- Gradual vision loss: Retinopathy or macular oedema or cataract.
Classification of Diabetic Retinopathy
Nonproliferative
- Background:
- Any of: microaneurysms, retinal haemorrhages, venous looping.
- Occasional cotton wool spots and hard exudates.
- Pre-proliferative:
- Any of: multiple dot and blot haemorrhages, venous beading, intraretinal microvascular abnormalities (IRMA).
Proliferative
- Any neovascularisation OR Vitreous haemorrhage OR Pre-retinal haemorrhage.
Macular oedema
- Clinically significant macular oedema:
- Retinal thickening/hard exudates within 500μm of fovea.
- Centre involving diabetic macular oedema.
Classification is important for risk stratification and subsequent management.
Management
The management options are chosen based on risk classification:
- Non-proliferative → Monitoring.
- Proliferative → Panretinal photocoagulation (PRP) of the retina.
- Clinically significant maculopathy (including oedema) → Macular grid laser.
- Diabetic macular oedema → Anti-VEGF or OZURDEX® (steroid implant).
If the patient also has cataracts, treat diabetic complications before cataracts are addressed.
Hypertensive Retinopathy
Chronic hypertension causes endothelial damage → atherosclerosis → constriction of retinal vessels → retinopathy.
Stages (compound on progression)

- Arteriolar narrowing.
- AV nipping OR silver wiring.
- Flame haemorrhages OR cotton wool spots.
- Disc swelling OR hard exudates OR retinal oedema.
Management
- Treatment is focused on targeting systemic hypertension.
- Patients with papilloedema and malignant hypertension need emergency assessment (discussed in detail in the Neuro-ophthalmology chapter).
Retinal Vessel Occlusions
Retinal arteries and veins can become occluded and cause vision loss. This section compares the different types of retinal vessel occlusion.
Key Presentations
Artery |
Features |
|---|---|
Central retinal artery occlusion (CRAO) |
Sudden painless loss of vision + RAPD + pale retina + Cherry red spot in macula. Irreversible infarction occurs within 90 minutes |
Branch retinal artery occlusion (BRAO) |
Sudden painless altitudinal visual field defect + swollen white retina along affected vessel. |
Obstruction of retinal arteries is considered a STROKE.
Vein |
Features |
|---|---|
Central retinal vein occlusion (CRVO) without ischemia |
Sudden painless loss of vision + dilation of all branches of CRV + dot/flame haemorrhages in all 4 quadrants + optic disc and macular swelling |
Central retinal vein occlusion (CRVO) with ischemia |
Sudden painless loss of vision + same signs as above + RAPD + rubeosis iridis |
Branch retinal vein occlusion (BRVO) |
Reduced vision (painless) + altitudinal visual field defect + retinal haemorrhages (commonly in superotemporal quadrant) |
The differentiation of these conditions based on clinical signs is both highly examinable and clinically important.
Retinal Artery Occlusion

An ophthalmic emergency which can lead to irreversible vision loss. THIS IS A STROKE.
Pathology
- Occlusion of the retinal artery → hypoxia of the retina → cell death and neovascularisation.
- Systemic causes of arterial occlusion apply just the same to the retinal artery, with the most common cause being atherosclerosis.
- Irreversible infarction occurs within 90 minutes of CRAO.
- The most common cause of BRAO is emboli.
Diagnostics
- Diagnosis is made clinically and is clear in the acute presentation but OCT can be useful in less clear cases and delayed presentations, where inner retinal atrophy can be seen.
- It is important to look for specific aetiology based on the presentation and look to treat underlying causes:
- 50-year-old woman with headaches → GCA?
- 70-year-old male smoker with diabetes and carotid bruit → carotid embolism?
Management
- Initial management of CRAO (within 24 hours): Ocular massage + IV acetazolamide ± AC paracentesis.
- No specific treatment for BRAO, but they should be urgently referred to the stroke team.
Around 30% of the population have a cilioretinal artery which provides anastomosis between the central retinal artery (supplying the inner 2/3 of the retina) and choroidal vessels (outer 1/3 of the retina).
Retinal Vein Occlusion

Retinal vein occlusion is the 2nd commonest retinal vasculopathy (to DR).
Pathology
- Occlusion of retinal veins can cause ischaemia, haemorrhage and oedema.
- It can lead to complications such as neovascularisation and oedema, which negatively affects vision.
Types
- CRVO → occlusion proximal to the lamina cribrosa.
- BRVO → occlusion of branch of central retinal vein.
- Ischaemic type is associated with a higher risk of neovascularisation and a poorer visual prognosis.
- Ischaemia is picked up by worse symptoms and additional ischaemic signs such as RAPD, rubeosis iridis and non-perfusion on FFA.
Diagnostics
- Patients are worked up for systemic risk factors for thrombosis including general bloods, diabetic screen and blood pressure. Keep a high index of suspicion for vasculopathies and thrombophilias in suggestive presentations.
- FFA is abnormal.
- OCT is useful to identify and monitor macular oedema (thick on OCT).
Management
- Treatment is guided by specific complications which in turn determine visual prognosis.
- Neovascularisation → Panretinal photocoagulation (PRP) laser (sectoral for BRVO).
- Macular oedema → Anti-VEGF or Ozurdex® (dexamethasone implant).
Ocular Ischaemic Syndrome
Angina of the eye caused by severe carotid obstruction.
Pathology
- Most commonly caused by atherosclerosis.
- As with other causes of ocular ischaemia, this can lead to neovascularisation of intraocular structures such as the retina and iris.
Diagnostics
Presentation
- The patient is typically an elderly male with a history of vascular risk factors such as diabetes, smoking and hypertension.
- Painful gradual reduction in vision with episodes of transient vision loss (amaurosis fugax) and orbital aching pain.
Investigations
- Examination might show flare in the anterior chamber.
Treatment
- Focused on relieving the carotid obstruction by stenting or endarterectomy.
Sickle Cell Retinopathy
More prevalent in patients of Afro-Caribbean origin. Different mutations of Hb determine the severity of disease. HbSS is associated with the worst systemic disease and HbSC is associated with the worst ocular disease.
Pathology
- Sickling of cells leads to occlusion and ischaemia. This can subsequently lead to proliferative changes and neovascularisation.
- There are 2 types: proliferative and nonproliferative.
- Severity of disease is determined by mutation, from mild to severe: HbSC → HbSThal → HbSS.
Diagnostics
Presentation
- Nonproliferative: Salmon patches (intraretinal haemorrhages) and black sunbursts (RPE hyperplasia).
- Proliferative: sea fan neovascularisation, vitreous haemorrhage and retinal detachment.
Investigations
- Diagnosis of Sickle cell is made by haemoglobin electrophoresis.
Proliferative sickle cell retinopathy is categorised according to the Goldberg classification.
Management
- Scatter laser photocoagulation can be used in severe sickle cell retinopathy.
Eales vs Coats Disease
These are 2 distinct retinal vascular diseases of unknown aetiology. They are frequently compared in exams.
Description |
Key Points |
|
|---|---|---|
Eales Disease |
Idiopathic retinal vasculitis |
Typically affects young Indian males Disease follows a course of inflammation → occlusion → neovascularization and vitreous hemorrhage |
Coats Disease |
Severe retinal telangiectasia that commonly affects young males. |
Presents unilaterally with:
|