A good way to approach uveitis is to treat it as a sign of underlying disease. Look for features that suggest inflammation of the uveal tract and then look for key features that point towards a particular diagnosis. You would've already covered many of these uveitic conditions elsewhere in medical school!
In practice, most cases of uveitis are idiopathic and no causes are found.
Uveitis Overview
The term uveitis describes the inflammation of the uveal tract, involving or not involving its neighbouring ocular structures such as the retina and vitreous. A wide array of diseases are known to cause inflammation of the uveal tract including infections, systemic inflammatory conditions and neoplastic syndromes. The disease course can vary significantly, acute or chronic, mild or severe, persistent or one-off. It largely depends on the underlying cause of inflammation.
Classification
Anatomically, uveitis is categorised in 4 ways:
- Anterior uveitis - Iritis + AC inflammation
- Intermediate uveitis - Pars planitis + vitritis
- Posterior uveitis - Chorioretinitis
- Pan uveitis - iritis + pars planitis + chorioretinitis (+ inflammation of associated structures)
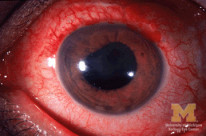
Anterior Uveitis

Overview
- Anterior uveitis is the inflammation of the iris (including pars plicata)
- Most commonly idiopathic, but can be HLA-B27 associated, infectious or systemic
- Anterior uveitis can predispose to posterior synechiae and angle-closure
- White blood cells can accumulate in the corneal endothelium and are known as keratic precipitates (KPs). The nature of these can be further classified based on appearance:
- Mutton fat KPs indicate granulomatous inflammation
- Stellate KPs indicate non-granulomatous inflammation
Presentation
- Inflammation of the iris and anterior ciliary body leads to AC flare
- Inflammation of the iris sphincter can lead to irregular miosis
- Typically presents with a painful red eye, AC flare, photophobia and blurred vision
Intermediate Uveitis
Overview
- Intermediate uveitis is the inflammation of the posterior ciliary body (pars planitis) and can also involve the vitreous
- Inflammatory accumulations in the vitreous are described as snowballs
- Characteristic white inflammatory exudation on the pars plana and ora serrata is described as snow-banking (can be seen on indirect ophthalmoscopy with scleral depression)
Presentation
- Painless blurry vision and floaters, without red eye
- Pars planitis and vitritis leads to floaters and blurring of vision
Infective Uveitis
Description |
Diagnostics |
Management |
|
|---|---|---|---|
Onchocerciasis (Onchocerca volvulus) |
|
Presentation
Investigation
|
|
Toxocariasis (Toxocara cani) |
|
Presentation
Investigation
|
|
Toxoplasmosis (Toxoplasma gondii) |
|
Presentation
|
|
Histoplasmosis (Histoplasma capsulatum) |
|
Presentation
|
|
Cytomegalovirus Retinitis |
|
|
|
Toxocariasis is an important cause of childhood leukocoria. The absence of calcification on CT scan differentiates it from retinoblastoma
Multisystem Uveitis
This section summarises some of the commonly examined causes of uveitis. It is important to be aware of these conditions for the exam.
Description |
Key features |
|
|---|---|---|
Sarcoidosis |
A multisystem inflammatory granulomatous disorder characterised by noncaseating granulomata |
Presentation
Investigation
|
Tuberculosis |
Multisystem Infective granulomatous disease caused by Mycobacterium tuberculosis |
Presentation
Investigation
|
Reactive arthritis |
HLA-B27 associated reaction caused by non-gonococcal infections, most typically chlamydia. |
Presentation
|
Behcet's Disease |
HLA-B51 associated multisystem vasculitis. |
Presentation
Investigation
|
Kawasaki Disease |
A medium vessel vasculitis of childhood |
Presentation
Investigation
|
Vogt-Koyanagi-Harada disease |
Multisystem granulomatous inflammation due to melanocyte Tcell hypersensitivity (commoner people with darker skin) |
Presentation
|
Tubulointerstitial nephritis and uveitis |
Non-granulomatous inflammation of the kidneys and the eye |
Presentation
Investigations
|
Juvenile Idiopathic Arthritis |
The most common cause of anterior uveitis in children. Also the most common rheumatological disease in children Non-granulomatous inflammation |
Presentation
|
Reactive arthritis was formerly known as Reiter's syndrome (redacted because Reiter was an SS officer who was found guilty of war crimes at the Nuremberg trials).
IVIg and high dose aspirin are used in the management of Kawasaki disease. Note that aspirin is otherwise contraindicated in children because it has been linked to Reye's syndrome.
Limited Ocular Uveitis
This section will summarise the important causes of uveitis which are limited to the eye without systemic involvement.
Description |
Diagnostics |
|
|---|---|---|
Sympathetic Ophthalmia |
T-cell mediated autoimmune granulomatous inflammation following traumatic insult. |
|
Birdshot Chorioretinopathy |
HLA-A29 associated uveitis with characteristic multifocal cream coloured oval lesions of the fundus |
|
Fuchs Heterochromic Uveitis |
Idiopathic anterior uveitis which also leads to cataracts and open-angle glaucoma Also known as Fuchs heterochromic cyclitis. |
|
HLA Associations
Many different types of HLA alterations have been associated with various ophthalmic diseases. Some of the more commonly examined associations are summarised in this section.
Disease |
HLA Types |
|---|---|
Acute anterior uveitis + reactive arthritis |
HLA-B27 |
Birdshot chorioretinopathy |
HLA-A29 |
Bechet’s diseases |
HLA-B51 |
VKH + sympathetic ophthalmia |
HLA-DR4 |
Multiple sclerosis |
HLA-B7, DR2 |
Sarcoidosis |
HLA-BA, B13 |

